neuroplex
New York Association of Neuropathologists
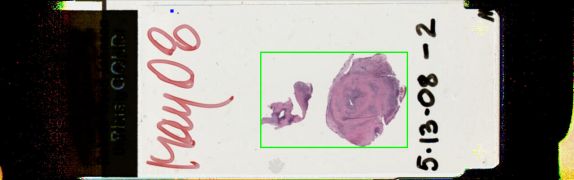
5/13/2008 Case 2: Syphilitic gumma
Presented by: Dr. Eric Richfield - Robert Wood Johnson University Hospital
Clinical History:
This 29 year old male had a first tonic-clonic seizure at work and a subsequent seizure in the ER. There were no other symptoms, nor neurological signs. There was a history of unprotected sex, but the patient was HIV negative, PPD negative, RPR negative and hepatitis A positive. FTA or other specific treponemal serology was not reported; CSF was not examined. Slit lamp examination was not done. An intraparenchymal mass, possibly attached to the falx, was completely resected. The patient was given Cepra. Penicillin was not given.
Sections showed a fibrotic lesion containing lymphocytes and plasma cells especially prominent around, and in the walls of, blood vessels. There was endothelial proliferation and recanalization, and occasional giant cells. These changes were interpreted as Huebner's arteritis/endarteritis obliterans. Spirochetes were not seen but it was noted that spirochetes are unusual in gummas.
Diagnostic Notes:
The diagnosis of syphilitic gumma was made.
Primary, secondary, latent and tertiary syphilis were reviewed. Gumma is a manifestation of meningovascular syphilis while infection of the brain parenchyma produces general paresis. Mixed forms can be seen and numerous other organs can be affected. Specific treponemal tests such as FTA are more expensive while the VDRL/
RPR testing is less expensive; false negatives are reported. Diagnostic criteria include pathology, presence of spirochetes, positive serology, response to penicillin and PCR testing.
Discussion centered on expanding the diagnosis of this interesting lesion in a patient where there is no serologic proof of syphilitic infection. Entities discussed in the differential diagnosis included MALT, Castleman's disease, plasmacytoma, infections, Rosai-Dorfman disease, Langerhans cell granuloma and lymphoma.