neuroplex
New York Association of Neuropathologists
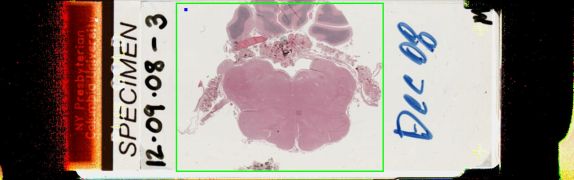
12/9/2008 Case 3: Anaplastic (WHO grade III) ependymoma
Presented by: Dr. Sharer - New Jersey Medical Center
Clinical History:
The patient is a 66 year old woman with intradural, extramedullary spinal masses, with evidence of thoracic spinal cord compression. She underwent resection of the thoracic lesion, followed in five days by resection of a separate cervical lesion. The submitted material was from the cervical resection, which had the same histology as the thoracic lesion.
Frozen section showed a tumor with pseudorosettes and uniform nuclei, which was well-demarcated and markedly hypercellular in some areas. There were also solid areas and some papillary areas. There were mitoses and anaplastic nuclei. The differential diagnosis included extra-axial ependymoma, possibly tanicytic, or anaplastic, and meningioma.
Work-up revealed a MIB1 which was low in some areas and up to 40% in other areas, consistent with two parts to the tumor. The cellular portion had a GFAP that was somewhat positive and a dot-like pattern on EMA staining, and was thought to be ependymal. The transthyretin staining was thought to be a red herring.
The second resection (cervical mass) showed the same histology, and the tumor made a ventricular lining at the edge, together with some ciliated cells.
Diagnostic Notes:
The diagnosis was Anaplastic ependymoma, WHO II, with zones of lower grade ependymoma.
Dr. Rosenblum stated that the jury is still out on the presence of focally increased cellularity and MIB1 in an otherwise Grade II ependymoma, and the WHO criteria are soft. Patient age and extent of resection are most important and there is no good neuropathological pattern.
It was also noted that NCAM (CD56) and e-cadherin are useful for the differential diagnosis of choroid plexus tumors (e-cadherin-positive) versus ependymoma (CD56-positive)