neuroplex
New York Association of Neuropathologists
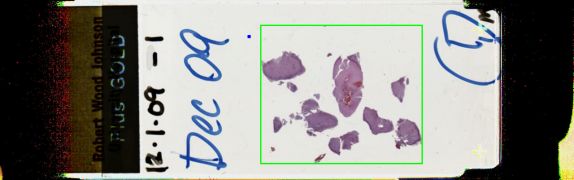
12/1/2009 Case 1: Neuroepithelial neoplasm, indeterminate grade
Presented by: Dr. Roy Rhodes - Robert Wood Johnson University Hospital
Clinical History:
A 48-year-old college admissions officer and fireman had a brief syncopal episode, which occurred while he was working in his firefighting capacity. This brought him to the Emergency Department, a few weeks prior to surgery. The ED workup found an enhancing laterally situated right temporal lobe mass, essentially thought to be incidental to syncope. The patient had had no headaches, no visual acuity change or blurred vision, no pain behind his eyes, no hearing change, no ear pain or discharge, no weakness, no bowel or bladder difficulties and no change in gait. Later neurological examination by the neurosurgeon was entirely normal. History showed a recent repair of a rotator cuff, wrist surgery a year previously, and a remote apparent lipoma resection in his thigh. He took alprazolam, vitamin B and omega-3. "Generally without fainting spells." MRI showed a 1.5 cm enhancing right posterior temporal mass with associated edema. The mass was lateral and said to be non-cystic and not dural based. CT angiography showed no relationship to any major blood vessels. The patient was given the option of following by observation or a resection, and he opted for resection. The operative report mentions that the operative bed following resection looked like normal white matter.
The tumor was well-demarcated. The tumor included papillary, spindle cells and angiocentric areas, and there was tumor in the subarachnoid space. Tumor invaded the dura. The larger cells stained as neurons and there were smaller cells. Nuclei had pseudoinclusions. There were up to 4 mitoses per one HPF, but overall, very few mitoses were present. There was some vasculitis and this was characterized as transmural with CD4+, CD8+ and CD45+ lymphocytes. Differential diagnosis included gangliocytoma, ganglioglioma, ependymoma (clear cell), PXA, neurocytoma and mixed glioma. Immunohistochemistry revealed that the tumor was EMA negative but many tumor cells expressed GFA; these were both spindly and small, but also large and binucleated. In the areas resembling Neurocytoma, synaptophysin was diffusely positive and NeuN stained both large and small cells; a few GFAP-positive cells were interpreted as reactive. Other areas also had strong synaptophysin-positive staining, including staining in the cytoplasm, and circumferential staining around ganglion cells. The perivascular spindle cells resembled tanicytic ependyma and had long GFAP-positive processes. The cells in the dura were GFAP-positive. A few cells expressed SMA and desmin and were interpreted as cross-reacting astrocytes, or possibly other cells such as neural crest derived myofibroblasts that are not part of the tumor; it was noted that we have little experience with these antibodies in brain tumors. A few cells expressed p53. MIB1 was 40%.
Diagnostic Notes:
The diagnosis was Neuroepithelial neoplasm, of indeterminant grade, without high-grade features, and with caution regarding prognosis because of the high MIB1, focal mitoses and dural infiltration. Possible sites of origin for this tumor include deep white matter, cerebral heterotopia, superficial granular layer (disappears at 18-20 gestational weeks), dural heterotopia, and neural crest. A primary leptomeningeal glioma should only be in the subarachnoid space, for proof of origin. A small primary parenchymal focus should be excluded to make this diagnosis (but that is possible in this case).
Cooper and Kernohan discussed theories of heterotopias and superficial glioma in 1951, including the possibilities of a pial defect, aberrant migration, separation and detachment from an outpouching of the telencephalic vesicle. Another idea is transformation of adult neural precursor cells from superficial stem cells which could produce a stem-cell-like glioma, and SVZ stem cells with mutations can make tumors in rodent cell cultures.
The vasculitis may arise from an attempt of the brain to repair itself. Endothelial cells release factors that stimulate glial growth (or overgrowth). Regarding the presence of myofibroblast-like cells, they could arise from neural crest via the meninges, the local blood vessel walls, circulating fibrocytes from bone marrow, or the could be an epithelial-mesenchymal transmission. In this case the myofibroblasts could be reactive.